The scope and purpose of GFI #152, remains the same as the initial document issued in 2003, but the regulatory body said the current version better aligns with today's scientific insights and clinical practices in human medicine.
Updates to the guidance include revisions to the risk assessment framework, updated ranking criteria for determining the degree of medical importance of antimicrobial drug classes, and a revamping of the ranking of antimicrobial drug classes as critically important, highly important, or important based on the newly updated ranking criteria.
In the original GFI #152, the US Food and Drug Administration (FDA) weighted its ranking criteria on drugs used to treat enteric pathogens caused by food-borne disease. “With improved scientific knowledge of antimicrobial resistance and medical advancements since 2003, FDA now believes the importance of an antimicrobial class should be ranked based on its use in human medicine, regardless of how a disease was transmitted. For that reason, the new criteria emphasize the utility of the drug to treat bacterial infections in humans, the seriousness of those infections, and the availability of alternative treatment options.”
Other proposed changes, it continued, include new text to address antimicrobial drugs that are not medically important (NMI), and updated exposure assessment tables based on extensive collaboration with the US Department of Agriculture’s Food Safety Inspection Service (FSIS) and Economic Research Service (ERS).
In terms of the proposed revisions to GFI #152, the agency said it considered feedback from its 2020 concept paper and public meeting on a potential approach for ranking antimicrobial drugs according to their importance in human medicine.
The FDA is accepting comments on the draft guidance for 90 days.
Sales of antimicrobials for farmed animals in the US
This month also saw the agency's Center for Veterinary Medicine (CVM) publish the latest data on antimicrobials sold or distributed in 2021 in the US for use in farmed animals.
The report shows that domestic sales and distribution of medically important antimicrobial drugs approved for use in farmed animals decreased by less than 1% between 2020 and 2021.
Since the significant decrease in sales volume in 2017, annual sales of medically important antimicrobials have remained at reduced levels. Compared to 2015, the peak year for sales, 2021 volumes decreased 38%, noted the publication.
“These sales and distribution data only reflect the total quantity of antimicrobial drug product that enters the market and does not represent how much or in what way these drugs are ultimately used. For instance, veterinarians and animal producers may purchase drugs in anticipation of using them but never actually administer them to animals, or they may use them in later years,” clarified the CVM.
US and Europe - a divergent policy approach
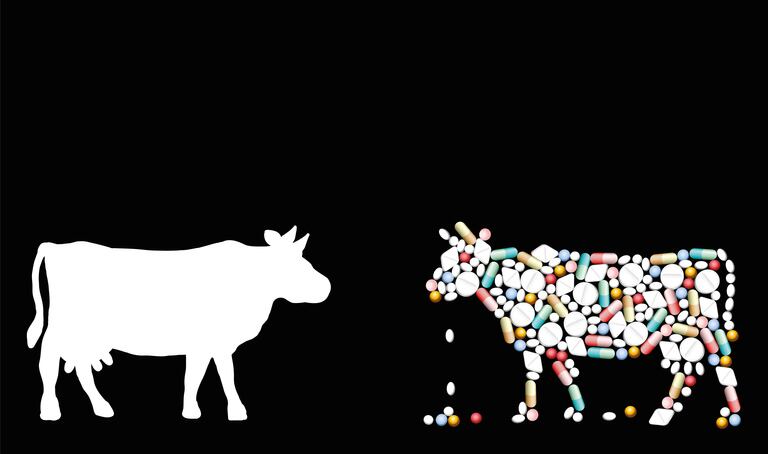
The extended use of low-dose antibiotics in feed for healthy animals creates ideal conditions for antibiotic resistant strains of bacteria to thrive, multiply, and spread into the human population, said the Natural Resources Defense Council (NRDC) in a new issue brief. “In fact, the science has long been clear that antibiotic-resistant bacteria do spread from livestock animals to human populations, including directly via the farmers and other workers handling those animals and indirectly through bacteria-contaminated water, soil, and air as well as on contaminated meats,” said the US based non-profit environment advocacy group.
The NRDC brief maintains that the US and Europe have taken divergent policy approaches to address the spread of dangerous antibiotic resistant bacteria, particularly in tracking and reducing antibiotic use in livestock production.
“Over the course of a decade, Europe’s explicit approach was aimed at improving animal health and preventing illness through changes to on-farm conditions and practices, thereby avoiding the need for antibiotics. That approach coincides with nearly all of Europe’s largest livestock producers reducing their intensity of antibiotic use by 50 to 60% between 2011 and 2020.
“European public health agencies, like the European Medicines Agency (EMA), played a crucial role in this reduction by building systems that collect and report data on veterinary antibiotic sales and usage. Those data are essential for tracking rates of antibiotic use and progress toward better antibiotic stewardship. US policymakers should learn from Europe’s experience and public health success.”
Use-reduction targets
The non-profit group said it has long urged three policies— modelled on Europe’s—that Congress or the FDA could implement without further delay.
One relates to setting ambitious use-reduction targets. “The FDA should set a goal of reducing livestock antibiotic use by 50% by 2025, relative to a 2010 baseline.”
The agency needs to also closely track antibiotic use in livestock production, said the advocates. “Robust tracking of antibiotic use is essential to measure improvements in antibiotic stewardship and progress toward national reduction targets. The public health need to robustly track antibiotic use, especially at the farm level, has been recognized in the US for decades but never acted on. This should be corrected at once. Simultaneously, the FDA should take immediate action to estimate annual antibiotic use in all food producing animals since 2009 on the basis of weight-adjusted national sales. This approach is endorsed by the World Organization of Animal Health. Our analysis already provides these weight-adjusted sales data. Ideally, however, the FDA would do its own weight adjustments, reporting them each December along with its annual sales summaries. Ultimately, public health goals will best be served if the US joins other countries in reporting national sales and/or use data using metrics that enable rather than obscure comparisons across countries or regions.”
Moreover, the US should end antibiotic use in healthy animals for disease prevention, added the NRDC. “Some of Europe’s major livestock producing countries discovered that an essential step to curbing the overuse of antibiotics was to end their use in healthy animals for so-called prevention purposes. Effective January 2022, these avoidable antibiotic uses became illegal across the EU with few exceptions. The new law also is consistent with 2017 guidelines published by the World Health Organization (WHO).”
The campaigners argue that evidence from Europe, to date, supported by published scientific reviews commissioned by the WHO, underscores that the use of preventive antibiotics is not necessary for animal health. In fact, it can be avoided through improvements made to farm practices and animal husbandry that help prevent disease from occurring in the first place, said the organization.